Navigating RSV disease: one family’s journey
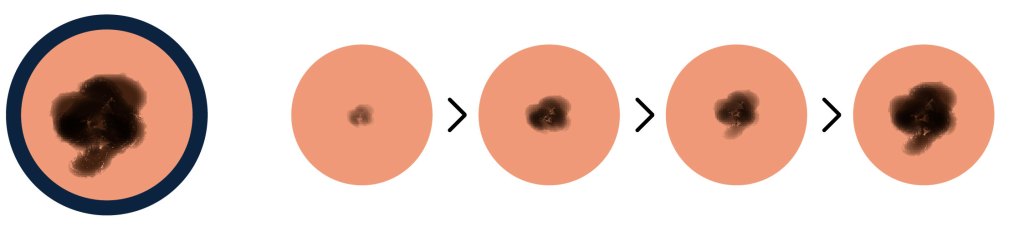
As the leading cause of hospitalization for infants in the U.S., respiratory syncytial virus (RSV) can progress to severe illness for some babies
June 11, 2025

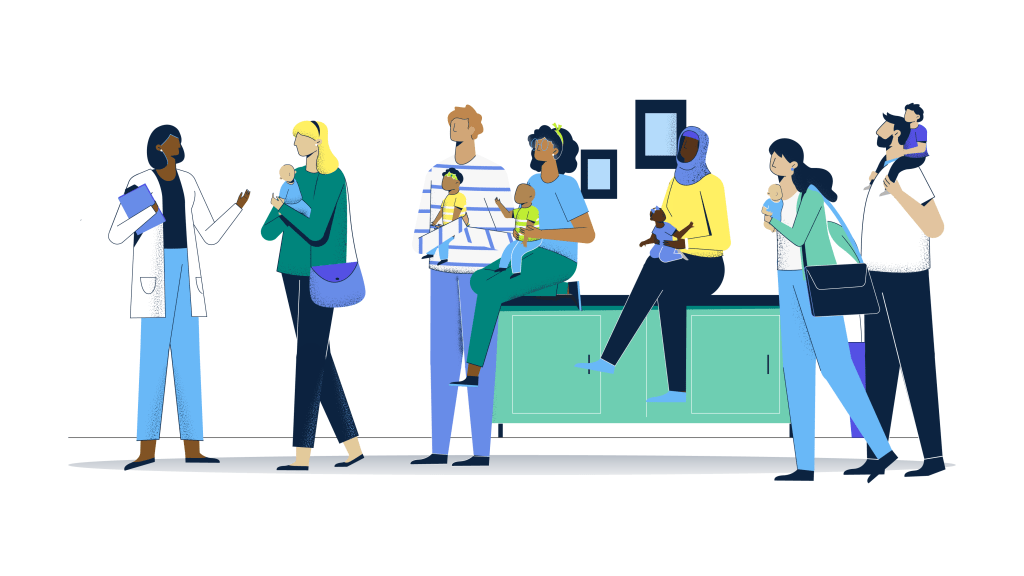
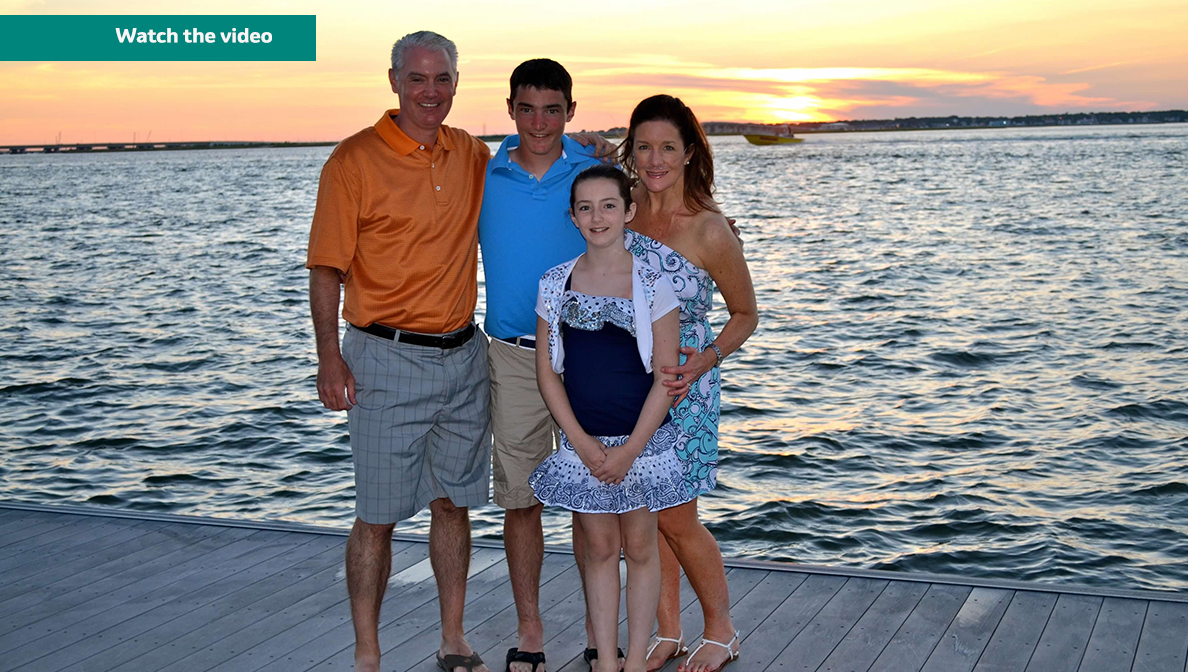
Caring for a child with respiratory syncytial virus (RSV) can be challenging. New parents Amanda and Jeremy thought they were as prepared as possible for any illness for their daughter Charlotte.

Charlotte’s first night in the pediatric ICU.
They had an established pediatrician, supportive family and friends and a variety of resources and supplies on hand to help manage symptoms. But they weren’t prepared for Charlotte to progress from having what they initially thought was a cold, with a cough and runny nose, to being admitted to the pediatric intensive care unit for RSV at only 7 months old.
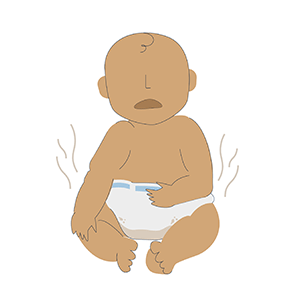
RSV is a contagious, widespread seasonal infection and the leading cause of hospitalization for infants under a year old in the U.S. Infants are among the populations most at risk of contracting the severe virus during their first RSV season, which typically starts in the fall and peaks in the winter in most regions of the U.S.
Charlotte’s experience with RSV
“Charlotte was a happy, chill baby. When she wasn’t happy, it was usually a sign that she was about to get sick,” said Amanda, who as a first-time parent hadn’t thought much about RSV up until that point.

On the day Charlotte was cleared to go home.
As Charlotte’s symptoms worsened, their doctor told Amanda and Jeremy what to look out for, mainly retracting or pulling in between and under the ribs, which was a sign of her struggling to breathe.
Amanda and Jeremy were surprised when Charlotte was admitted for difficulty breathing due to RSV and stayed in the pediatric ICU for a week.
Fortunately, she recovered and Amanda and Jeremy were so appreciative of her medical care. Today, Charlotte is a healthy and happy 3-year-old who loves spending time with her parents and younger brother.
Amanda understands that her family’s experience is unfortunately not unique.
"I urge all parents to understand the signs and symptoms of RSV so you can be prepared."
— Amanda
The impact of RSV on infants
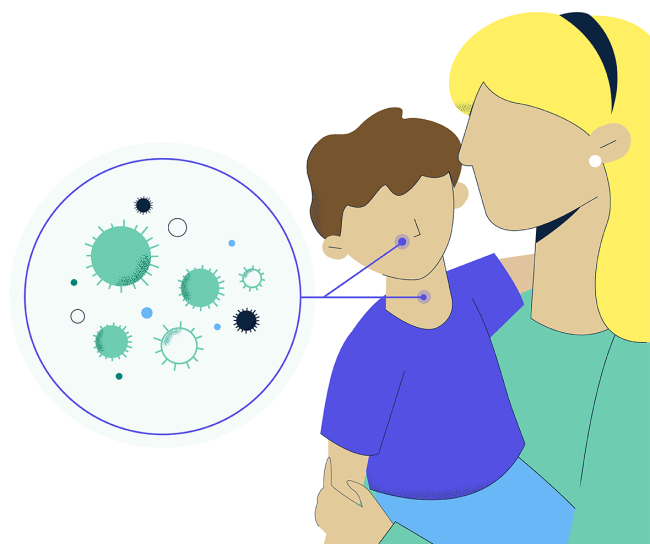
RSV is a common seasonal respiratory infection that can be spread through virus droplets when an infected person coughs or sneezes, or through direct contact with the virus, like kissing the face of a child with RSV.
It’s the most common cause of hospitalization in infants under one year old in the U.S.
Common symptoms include a runny nose, fever, coughing and wheezing. While RSV doesn’t usually cause severe illness, healthy and at-risk infants can develop more severe cases that may lead to illnesses such as bronchiolitis (inflammation in the small airways of the lungs) or pneumonia (infection of the lungs) and may require hospitalization.